An Introduction to Working with Functional Neurological Disorders
for:
North Staffs Aspiring Psychologist Group

Dr. Chris Gaskell
Senior Clinical Psychologist
Neuropsychology
North Staffordshire Combined Healthcare NHS Trust
Disclaimers
Emotionally pertinent areas 😦
Potentially distressing videos 📹
I’m learning too1 🧑🎓
Background
Terminology
FND = Functional Neurological Disorder.
- Umbrella Diagnosis ☔.
Subtypes include:
- FDS= Functional Dissociative Seizures (aka NEAD [Non Epileptic Attack Disorder] and others).
- FMD = Functional Movement Disorder.
- FCD = Functional Cognitive Disorder.
- Functional Stroke.
- Functional Tics.
- And many others.
Diagnoses:
Functional Neurological Symptoms Disorder (DSM-V)
Inclusion term to Conversion Disorder
Diagnosis requires motor and/or sensory findings.
Evidence of incompatibility between symptom and recognized neurological/medical conditions (APA, 2013, Stone et al., 2010b).
Symptoms must impair social/occupational functioning or lead individuals to seek a medical opinion.
No duration or severity criteria, or explicit rules for exclusion based on additional symptoms.
Dissociative Neurological Symptom Disorder (ICD-11)
- Much push back on terminology from FND charities and specialists around the world.
Videos of FND
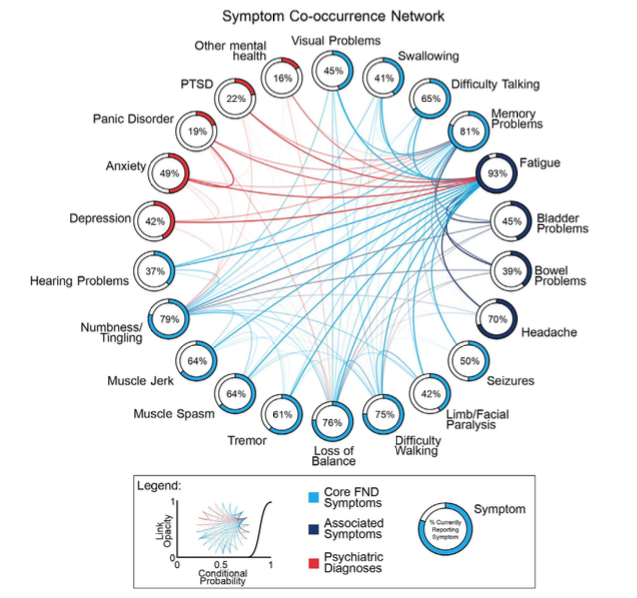
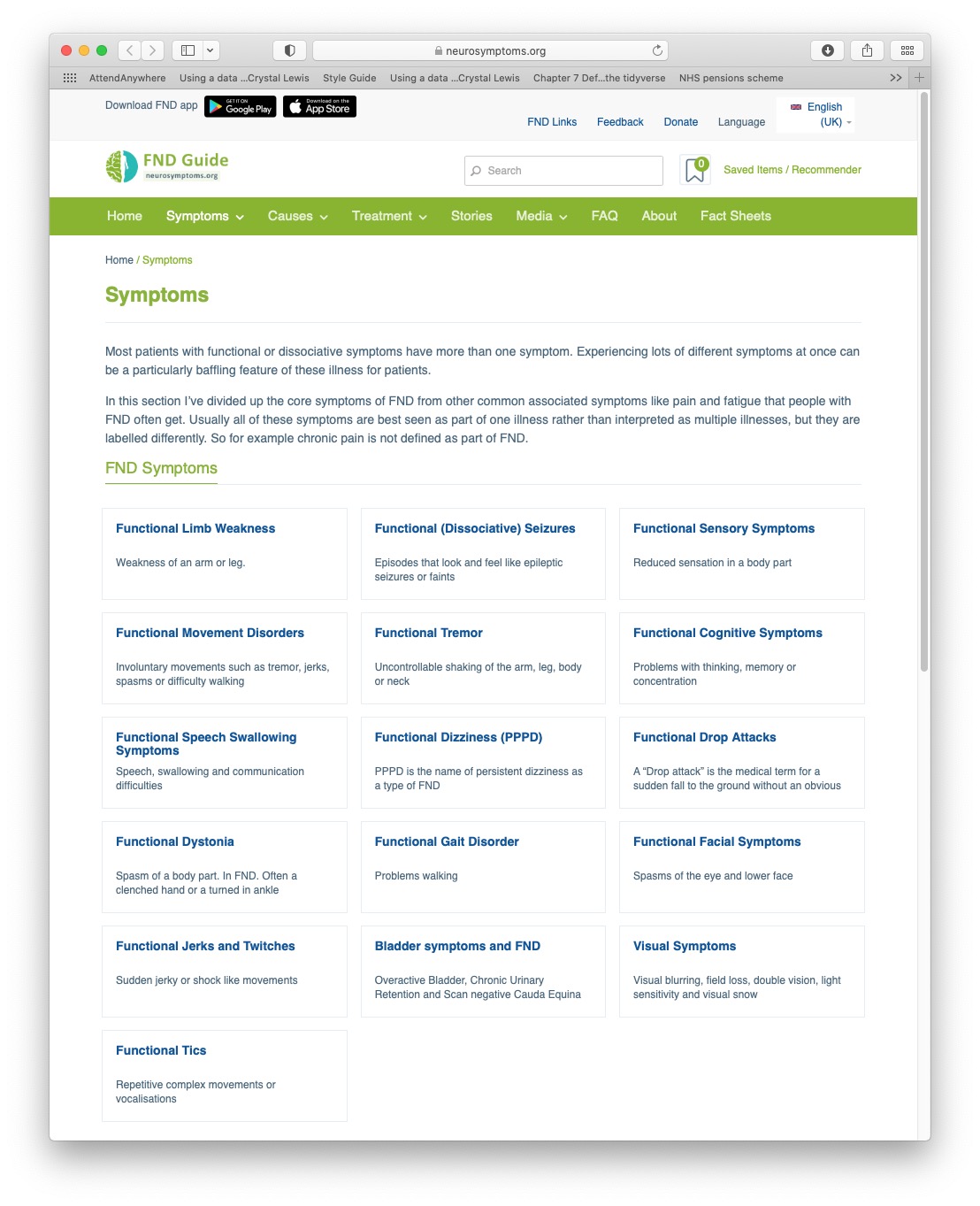
Symptom Heterogeneity
Classified by neurosymptoms.org, extracted 2021
Functional vs. Organic
Functional = Impairment of function.
Not suggesting a behavioural or intentional component.
Functional vs. Organic debates are outdated and inaccurate dualism.1
Can a person be non-organic?2
Software problem vs. hardware problem?
Diagnosis, Prevalence & Terminology
Important Notes around Diagnosis in FND
Based on positive clinical signs/symptoms1.
Internal inconsistency (reversibility) and/or to a lesser extent incongruency with known patterns of structural neurological disease.
Trauma is not required for diagnosis (more on this later).
Perceptions of ‘diagnosis of exclusion’ and hesitancy lead to damaging delays in diagnosis.
Following diagnosis, new symptoms are frequently (and wrongfully) dismissed.
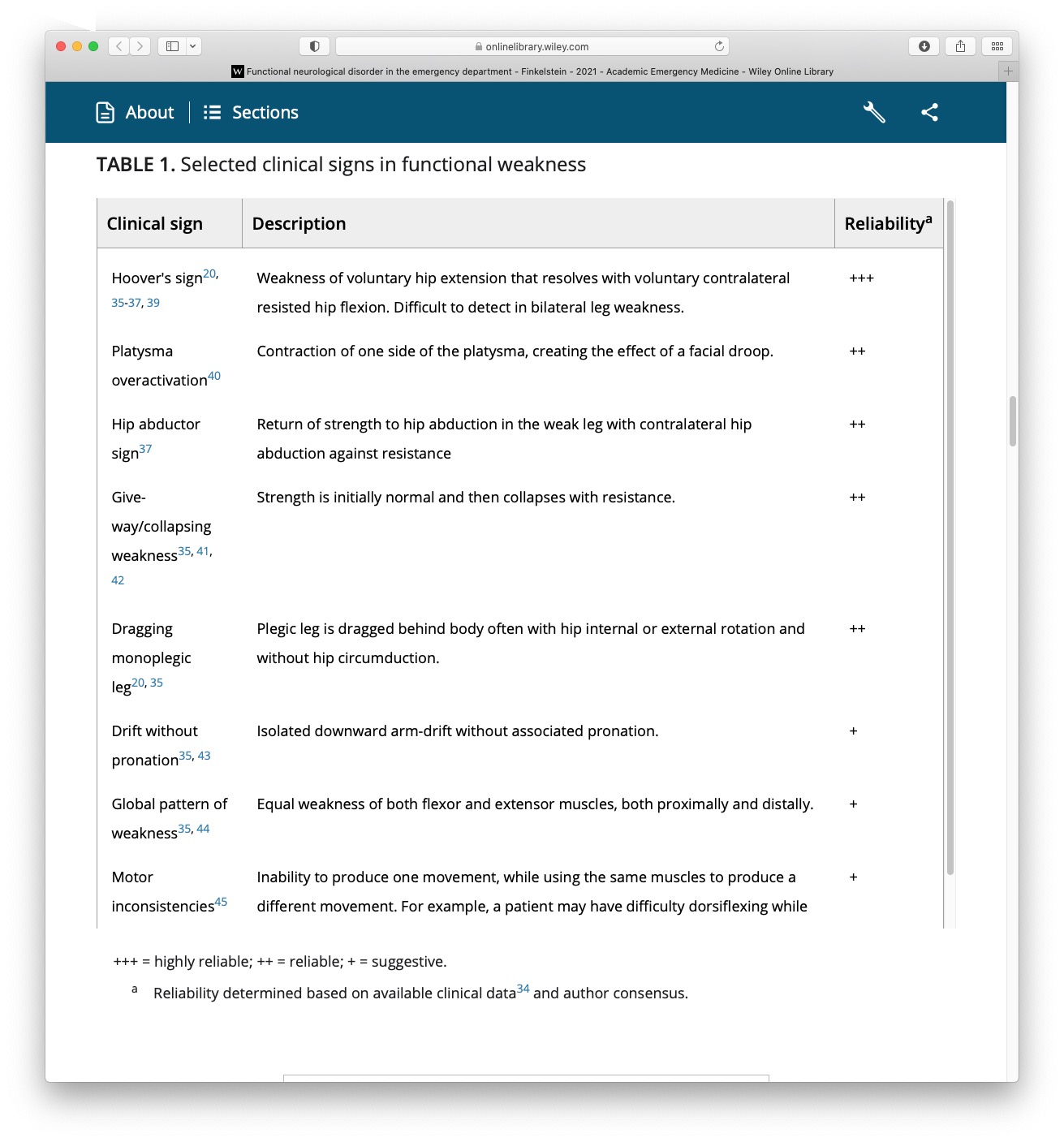
Symptoms: Functional Movement
Taken from: FND in the emergency department Finkelstein et al (2021)
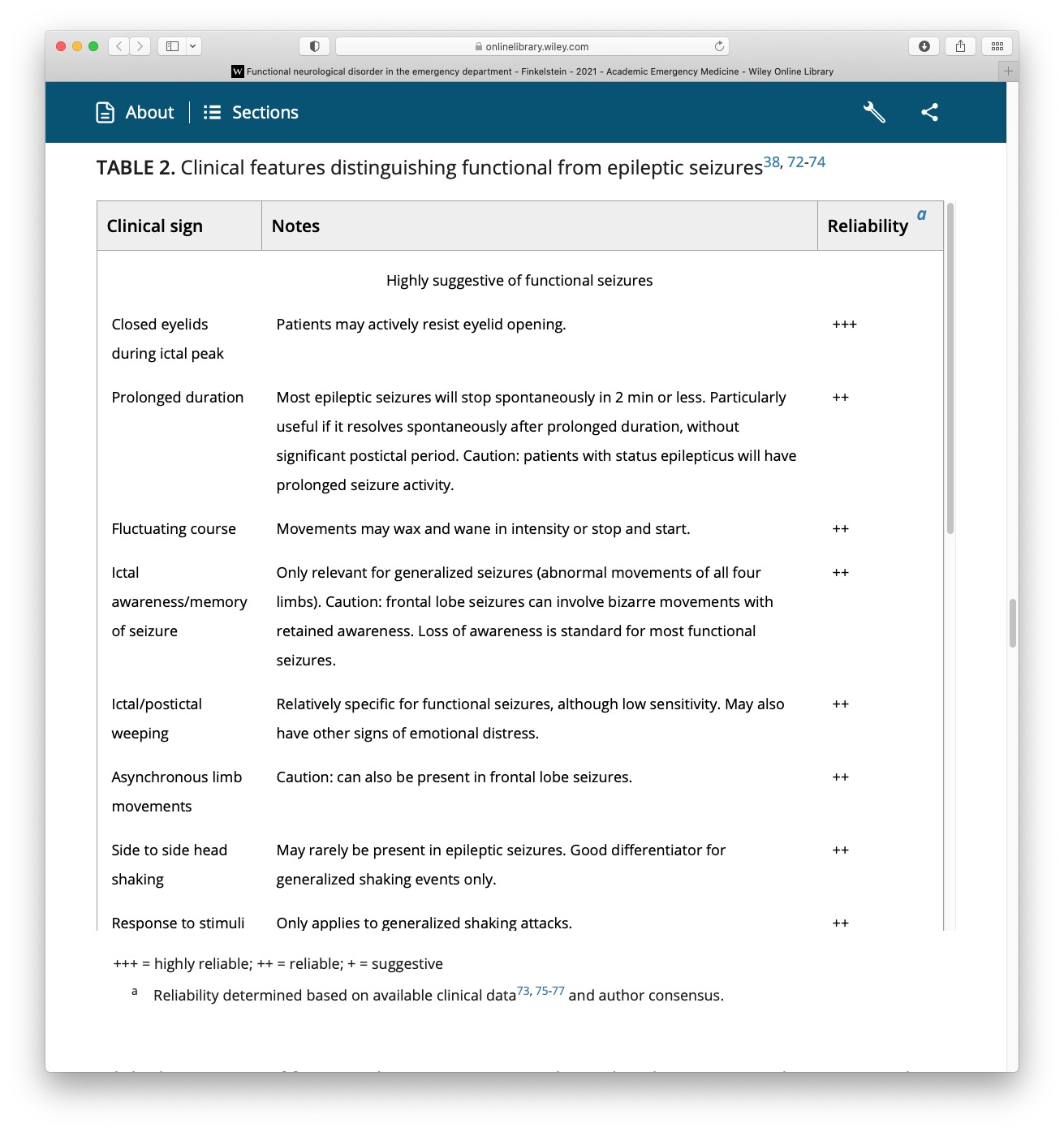
Symptoms: Functional Seizures
Taken from: FND in the emergency department Finkelstein et al (2021)
How Common Is FND?
FND Prevalence: 50/100000 in the population (Carson, 2016).
Functional Seizure Prevalence:
2-33/100000 (Carson, 2016).
Recent estimate = 24/100,000 (Norway) (Villagrán, 2021) .
Estimated 20,000 people in the UK.
8-12% of new presentations to seizure clinics (Angus-Leppan, 2008).
11% of seizures presenting to emergency services (Dickson et al., 2017).
What Are The Risk Factors For FND?
Age:
Presents across the life span.
Young adults (15–19) most at risk: 59.5 per 100,000. (Villagrán et al., 2021)
Gender:
Female preponderance = 60-80%.
Disparities less evident in older cohorts (e.g., Jungilligens, 2021)
Epilepsy: High rate of co-morbidity.
Learning Disabilities: High rate of co-morbidity (Rawlings et al., 2021).
Demographics:
- White and low SES
What Are The Risk Factors For FND?
Psychiatric Co-morbidity:
Anxiety and depression.
Interpersonal disorders.
PTSD, Trauma.
Health Co-morbidity:
Pain & Fatigue.
Sleep disturbance.
Migraine.
TBI.
Epilepsy Surgery
Misdiagnosis & Delayed diagnosis
Difficult at times to distinguish from other conditions.
Often leads to problems with:
Journey to diagnosis can be very long. When using gold standard assessment (VT) mean duration of 8.4 years (median = 3) (Kerr et al., 2021)
Response to functional seizures with seizure protocols (very common, see Jungilligens et al., 2021).
Prolonged use of anti-convulsants.
Lack of access to necessary support.
Time to receive treatment even longer.
Terminology and Language
Many terms have been used:
Non-epileptic attacks.
Psychogenic seizures.
Psychogenic non-epileptic seizures (PNES).
Dissociative seizures.
Conversion disorder.
Functional seizures.
Psychological seizures.
Pseudo-seizures.
Labels Matter
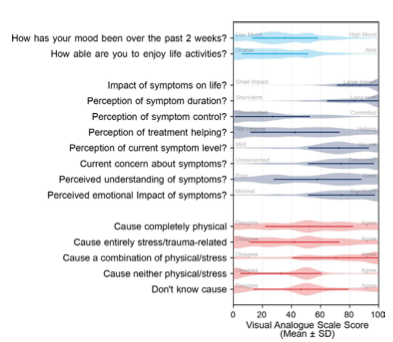
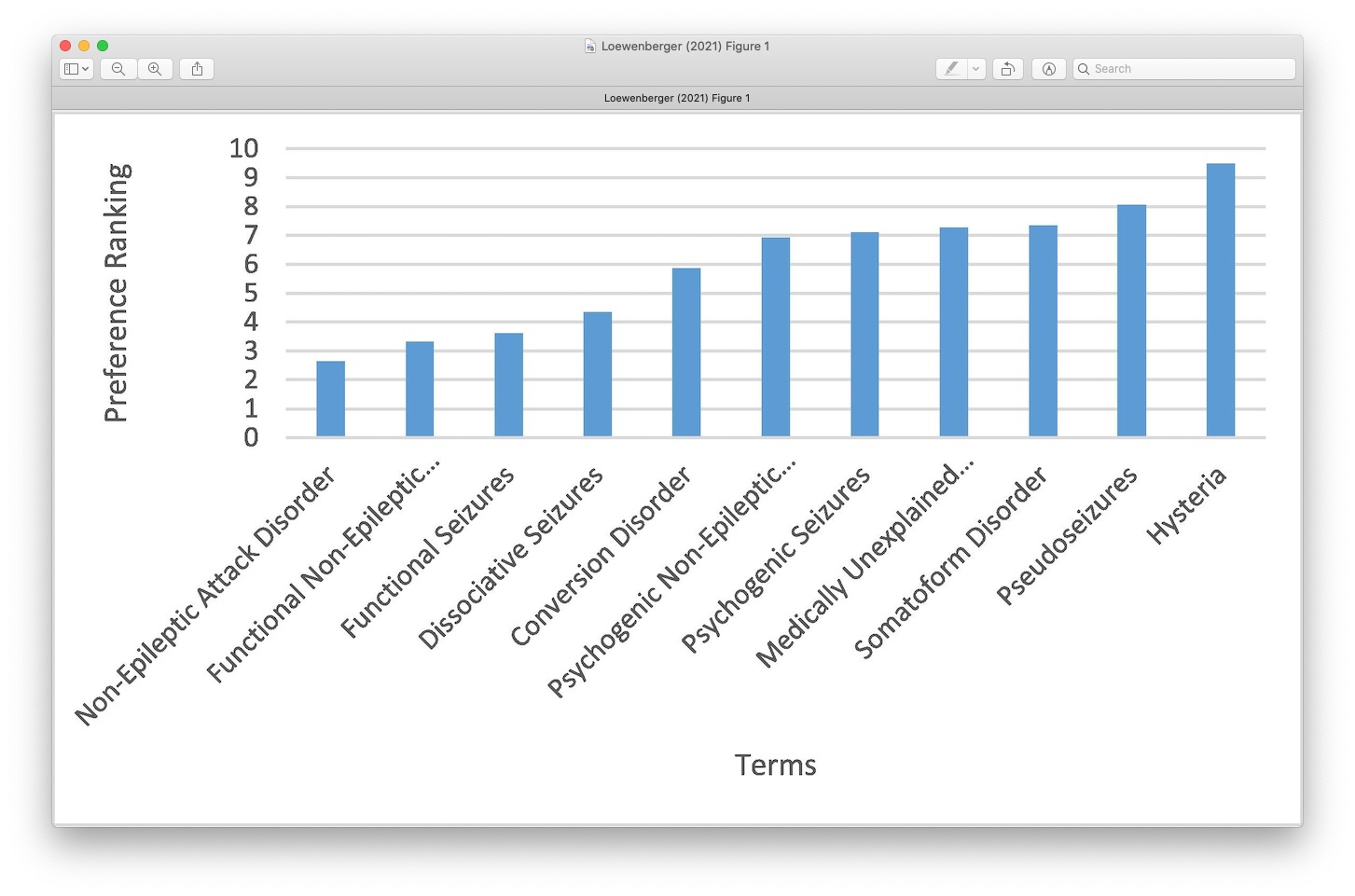
What do Patients Prefer?
Taken from recent Loewenberger, 2021 (UK service evaluation)

Not to be Confused With
Malingering: Deliberately manufacturing symptoms for material gain e.g. Money.
Factitious Disorder: Deliberately manufacturing symptoms for emotional gain e.g. Attention.
Do not mistake symptoms for factitious/malingering just because it doesn’t fit with what your framework.
FND is not Malingering! (see Edwards et al., 2023)
Theory
The Mind Body Link
Psychological experiences influence the body All The Time.
The cause is not medical but the impact on the body is real.
Sudden shock = heart beats faster.
Embarrassment = face goes red.
Upset = eyes produce tears.
It is normal for changes to happen in the body without a medical cause or disease.
FND also happens through this Mind-Body link.


Autonomic Reactions
Fight/flight/freeze response - evolutionary based fear response that is adaptive for survival.
Freezing is one of the main defensive threat reactions across species
Parasympathetic branch of the nervous system.
A means of responding to a threat or a trigger (at times adaptive)
Trauma
Traumatic event: incident causing physical, emotional or psychological harm.
Single event or repeated incidents (i.e., complex).
Recent or a long time ago.
Highly common in FND (compared to case controls, Ludwig et al., 2018).
Does not consistently explain aetiology or onset.
Not always helpful to ask.
Be careful with the notions of conversion. It may be relevant for some but not all.
Rates of Stressful Life Events
Taken from recent Ludwig et al 2018.
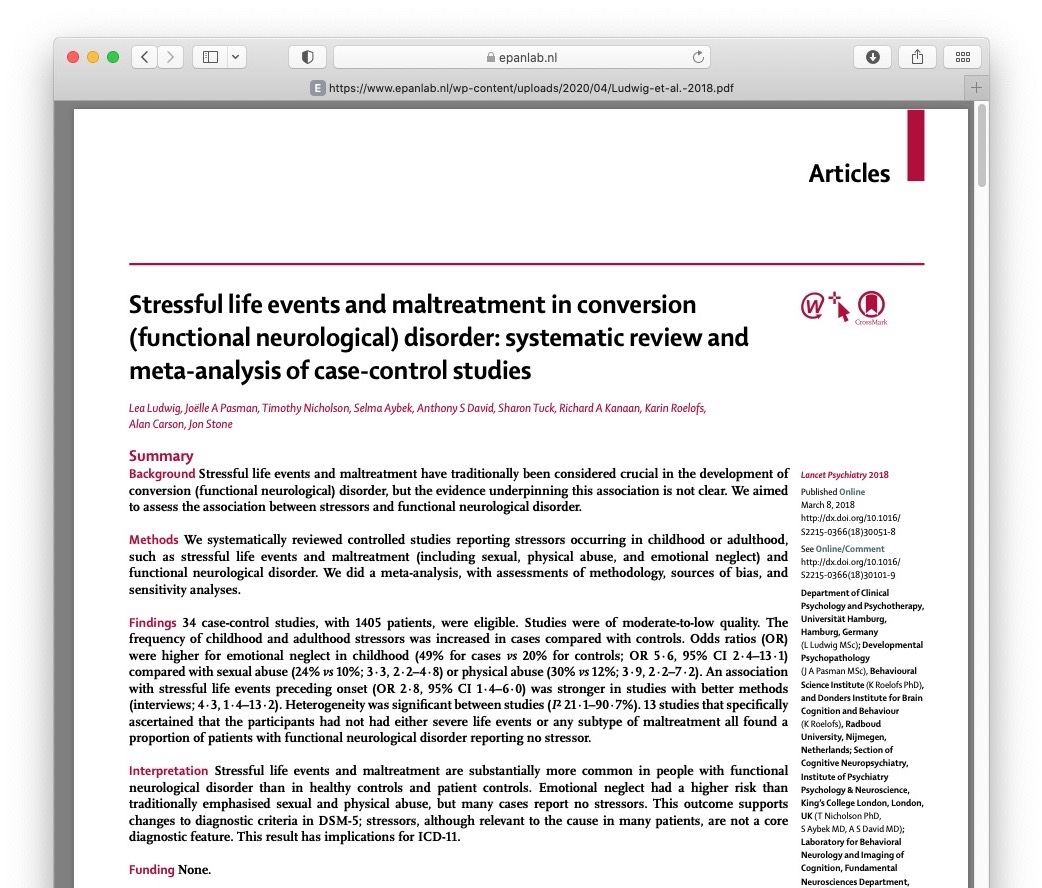
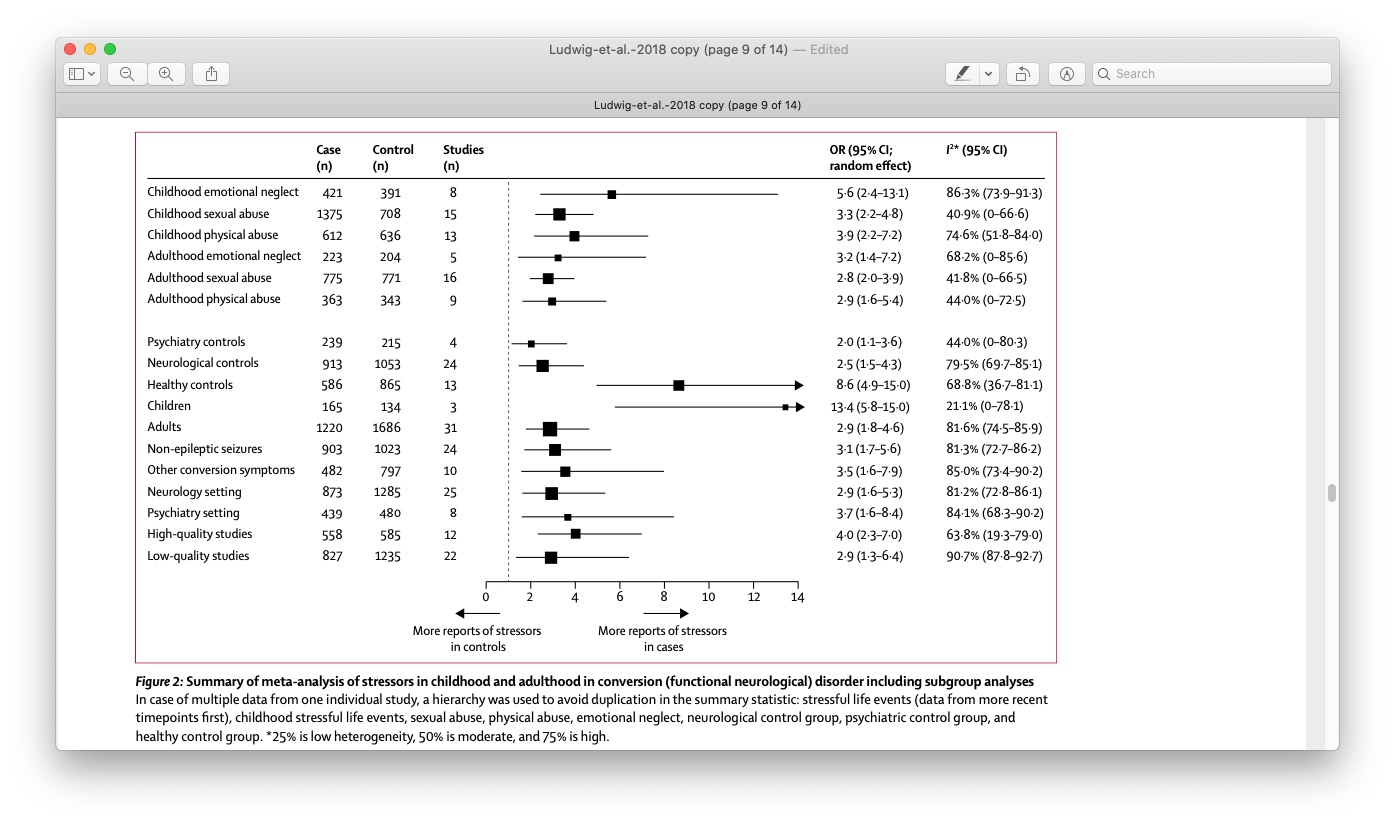
Important Point
Although Rates are high, many people with FND do NOT report having experienced any trauma.
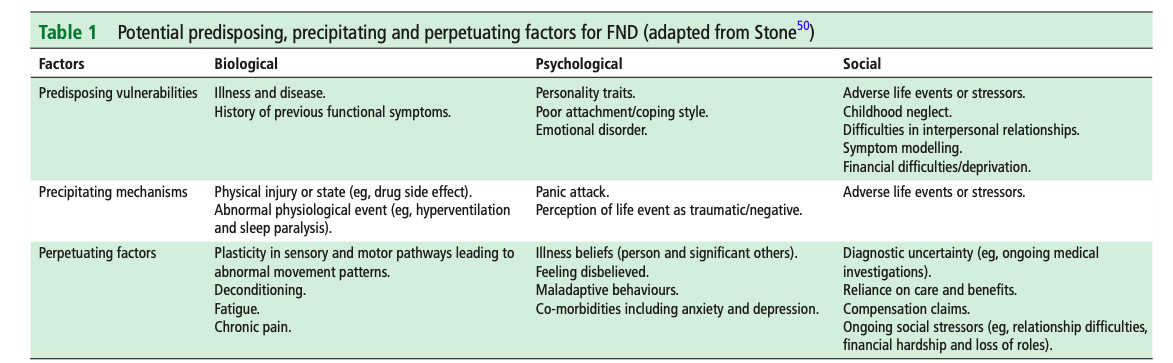
Biopsychosocial & 3 Ps
Taken from Reuber 2009
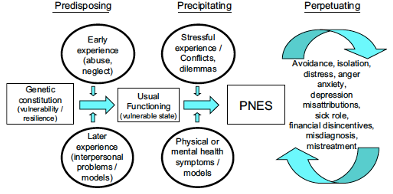
Taken from Nicholson 2020
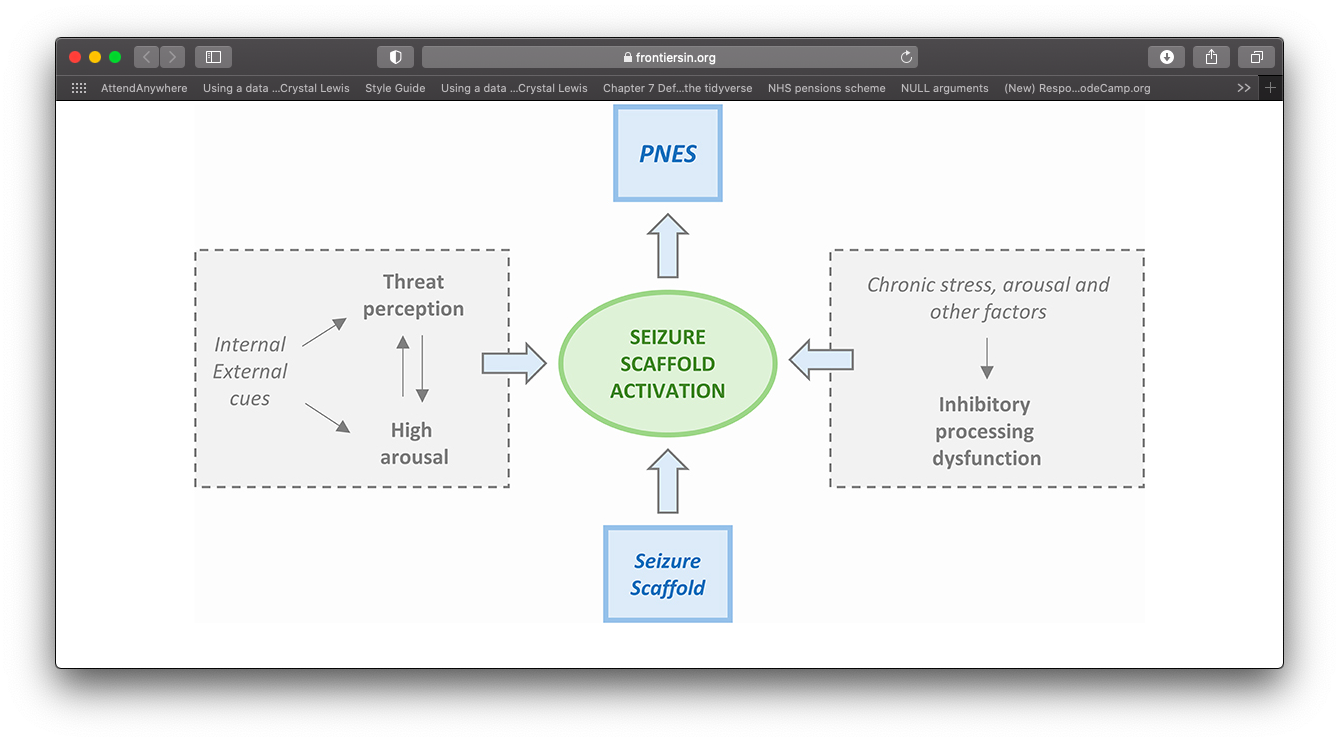
Integrated Cognitive model
Model proposed by Reuber & Brown (2017)
Single explanatory framework.
Helps to account for variation in psychological history.
Symptoms = FND scaffold + breakdown in inhibitory processes.
Brain response to sensory input provides error.
Scaffold becomes activated (e.g., by arousal, emotions, thoughts).
Over time this becomes a conditioned response.
Wilful submission.
Integrated Cognitive Model
Taken from Anzellotti et al., 2020 (Based on Reuber & Brown)
Predictive Processing Errors
Treatment Approaches
What Treatment is Indicated?
It depends on the person.
Heterogeneity requires idiosyncratic approach.
For many patients, treatment will require MDT input.
Clinicians with familiarity in FND.
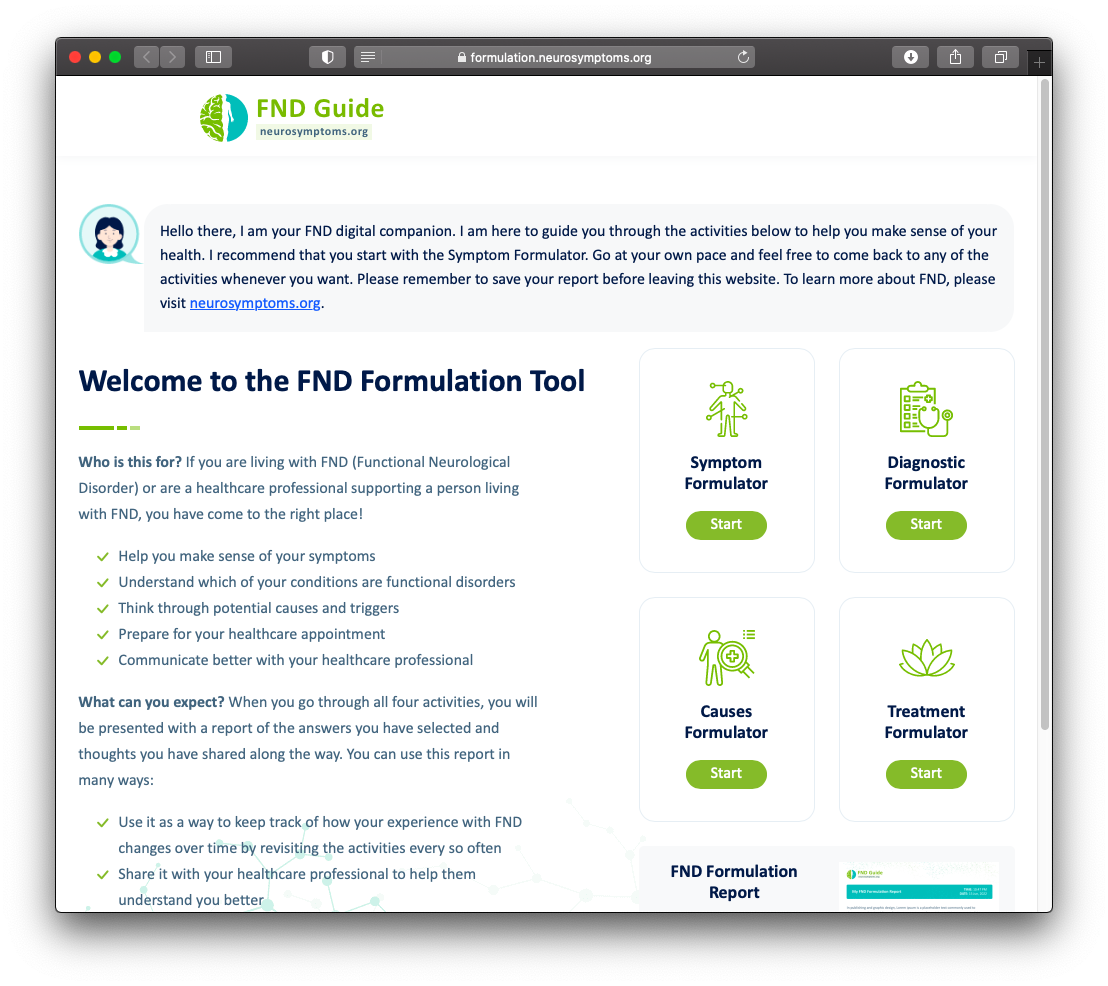
NeuroSymptoms: Treatment Formulator
Support patients to use the newly developed tool from neurosymptoms.org
Role of Psychology
Potentially suited to help all FND variants (won’t be necessary for all).
Co-morbidities needs to be accounted for.
Treating underlying and potentially long-standing distress (e.g., anxiety, depression, trauma).

The Evidence Base?1
Psychology
Few RCTs.
Systematic reviews support psychotherapy for FND (Gutkin et al., 2021).
47% patients achieve seizure freedom (Carlson & Perry, 2017).
Recent RCT however found no significant change for seizure frequency (CODES, 2020).
Neuro-Stimulation
- Small but emerging evidence base (Gonsalvez et al., 2021 for a review).
Physiotherapy
- Preliminary feasibility for physiotherapy (Maggio et al., 2019).
Acceptability
Some patients ambivalent to treatment.
Doesn’t always fit with patient view of difficulties.
Comes following a long journey.
High expectations.
How do Treatments Work?
Multi-faceted.
Relevant mechanisms of change across all therapeutic approaches.
Psycho-education likely to be important.
Ample evidence that CBT helps in the short term.
Trauma focused work important (if needed).
Approach should be tailored (see Myers et al., 2021 for a guide).
Resources
Websites
FND Hope
FND charity
Lots of helpful information and resources for patients.
FND Society
Professional network for FND
High quality teaching and educational material.
Manchester Neurosciences (Salford NEAD service)
NEAD service website
Information and clinical resources for patients and clinicians.
Neurosymptoms.org
Informational website for patients and professions
Lots of high quality resources and information sheets
Thanks for Listening !
FND for North Staffs Aspiring Psychologists